Dual Diagnosis Treatment for Depression and Substance Addiction Recovery in Los Angeles, CA
Dual Diagnosis Addiction and Depression Treatment Los Angeles
At Harmony Place, we take a compassionate and personalized approach to dual-diagnosis treatment, offering specialized care for depression and substance abuse across our three Los Angeles facilities. We know that depression and addiction often go hand in hand, and lasting recovery requires addressing both conditions simultaneously. Our full continuum of care is designed to support you at every stage of your healing process, providing the tools and resources you need to regain balance and reclaim control of your life. For those seeking depression treatment in Los Angeles, our facilities offer a calm, supportive environment where your well-being is our top priority.
Our treatment programs are tailored to meet your unique needs, combining evidence-based therapies and compassionate care to create a path toward sustainable recovery. At Harmony Place, you’ll have access to a wide range of therapeutic options, including individual counseling, group therapy for peer connection, and cognitive behavioral therapy (CBT). These therapies are proven to help with both addiction and the symptoms of depression. Whether you’re exploring inpatient depression treatment in Los Angeles or looking for outpatient options, our programs are designed to address the underlying causes of your mental health challenges while supporting your long-term sobriety.
To make treatment as accessible as possible, Harmony Place accepts most health insurance plans and offers guidance in verifying your coverage for dual-diagnosis programs. Whether you’re searching for a depression treatment center in California or a trusted facility for dual-diagnosis depression in Los Angeles, our team is here to help you take the first steps toward freedom from addiction and depression. Contact us today to learn more about your treatment options and how Harmony Place can guide you toward renewed hope and lasting recovery.
Available Depression Treatment and Therapy Options in Los Angeles, California
Depression significantly differs from normal feelings of sadness or grief. People go through difficult times, and negative feelings come and go. It is not uncommon to hear people describe themselves as being depressed when grieving a loss, such as a breakup or the death of a loved one. They might also feel this way following significant changes in life, such as childbirth or moving to a new city.
In some cases, the feelings they have are normal grieving responses. However, sometimes, they might be signs of a depressive disorder. One must understand the difference between depression and grief to provide the best care possible for those who struggle with either or both.
Harmony Place offers depression treatment interventions in Los Angeles, California, for those who struggle with their mental well-being.
What Is Major Depressive Disorder (MDD)?
Major depressive disorder (MDD) is not a medical condition that should be taken lightly. It often affects the way people think and behave. It is also called depression. Major depressive disorder is treatable. With the right therapy and a sound support system, people can come out of depression.
Depression is characterized by loss of interest in previous hobbies, disappearing for long periods, and other symptoms that could affect one’s ability to perform their duties at home and work and could lead to other mental and physical challenges.
What Are the Signs of Major Depressive Disorder?
While sadness and constant tiredness or lethargy could be signs of depression, there are other things to look out for. Most people with depression make efforts to conceal their symptoms from their families and others around them. On the other hand, some do not recognize that they are depressed. Depression can be diagnosed based on how long a person has been faced with the signs and symptoms attributed to depression.
Some of the significant signs that could be seen in persons struggling with depression include the following:
Constant Feeling of Tiredness
People who have difficulty sleeping are a lot more likely to develop depression than those who get enough sleep. Alternatively, a lack of sleep or insomnia can be a sign of depression. Sleeping too much can also be a sign of depression.
Withdrawing from Friends and Family
People with depression sometimes disappear for long periods without communicating with their friends and family. This could be because they feel ashamed of their vulnerability, are scared to show “weakness,” or simply because they cannot muster enough energy to engage in conversations.
Change in Appetite or Diet
Certain people with depression turn to food for solace, while some have a decreased appetite because they no longer feel any form of interest in or zest for life.
Strange Body Pains
Although MDD is a mental disorder, there may be physical affectations in people who have this disorder. They often complain of joint pain, back pain, muscle aches, headaches, and digestive issues that come out of nowhere and do not respond to treatment.
Being Easily Distracted
People with depression usually find it hard to concentrate on the things they have to do and often find themselves losing their train of thought or getting lost in conversations. It is possible that they also present with memory loss.
Increased Levels of Drug and Alcohol Use
When individuals have symptoms of depression, they sometimes feel the urge to numb their feelings of sadness, levels of anxiety, or loneliness. This makes them more susceptible to becoming addicted to drugs or alcohol. Also called “self-medicating,” this is a common maladaptive coping mechanism for mental health disorders.
Recurring Suicidal Thoughts
Someone who suffers from depression sometimes may begin to joke about death or dying. They may begin to talk about suicide or death more often than usual. It does not matter if they plan to act on these thoughts or not.
Sometimes the symptoms of depression are subtle and hard to notice until one day, they realize that their home is cluttered and disorganized. Or they have not been to work for days or even showered.
If you or any of your loved ones present with one or more of these symptoms and they have persisted for two weeks or more, prioritize your mental health. Visit us at Harmony Place to learn more about the treatment options available, or take our free personality disorder assessment, to see if our depression treatment center in Los Angeles is right for you.
How to Treat Depression
Depressive disorders sometimes come with deep feelings of hopelessness. There are several forms of therapy that can be used to deal with depression and facilitate recovery. Depending on the underlying causes of depression, one type of therapy might be better than another.
Psychotherapy
Psychotherapy has been shown to be an effective treatment for people suffering from depression and other mental conditions.
Psychotherapy is frequently used combined with pharmaceutical treatment. There are numerous types of psychotherapy, and some people respond better to one than another. Finding the one that properly addresses the patient’s needs and poses the least threat is essential.
Cognitive Behavioral Therapy (CBT)
During CBT, a therapist will work with the patient to uncover unhealthy patterns of thought and identify how they may be causing them to have harmful behaviors, reactions, and beliefs about themselves.
Dialectical Behavior Therapy (DBT)
DBT focuses on validating or accepting uncomfortable thoughts, feelings, and behaviors rather than fighting them.
What Is a Dual Diagnosis Or a Co-Occurring Disorder?
Dual diagnosis, also known as a co-occurring disorder, happens when you experience both a mental health disorder, like major depressive disorder (MDD), and a substance use disorder at the same time. These conditions often influence one another, making treatment more complex. For example, you might struggle with a depression disorder while also dealing with drug addiction or alcoholism.
When you have a dual diagnosis, it’s important to address both issues simultaneously. Treating one without the other can lead to incomplete recovery. With specialized care, you can work on managing your psychological distress while overcoming substance abuse. This concurrent treatment for substance use and depression helps you achieve lasting recovery and better overall well-being.
What Do Co-Occurring Depression and Addiction Treatment Programs Include?
Co-occurring clinical depression and addiction treatment addresses both conditions simultaneously, recognizing how they interact and affect your overall well-being. When you struggle with depressive symptoms, it can lead to or worsen substance abuse, and addiction can intensify feelings of sadness, hopelessness, and isolation.
For Co-occurring substance addiction and depression treatment, you receive support for both mental health and addiction through therapies like Cognitive Behavioral Therapy (CBT), individual counseling, and addiction support groups. This integrated approach helps you tackle the root causes of both issues, guiding you toward healthier coping strategies for depression and addiction. By treating addiction and depression together, you have a better chance at long-term addiction recovery and improved mental health.
Statistics on Depression and Substance Abuse in Los Angeles, California
From Feb. 1 to 13, 2023, 31.7% of California adults reported symptoms of anxiety and/or depressive disorder, according to KFF. In 2019, 58.5% of California’s substance use disorder treatment facilities provided programs for those with both co-occurring mental health concerns and substance use disorders, as reported by the California Health Care Foundation.
In 2018, 19.3% of U.S. adults with a mental illness, or 9.2 million people, also had a substance use disorder, according to NAMI California. The 2022 National Substance Use and Mental Health Services Survey by SAMHSA identified 931 facilities treating clients with co-occurring conditions. Mental Health America ranked California 16th lowest in the U.S. for prevalence of mental health and substance use issues.
What Is Los Angeles Best Known For?
Los Angeles is best known for its blend of iconic landmarks, entertainment, and cultural attractions. In the heart of the city, you’ll find the Hollywood Walk of Fame, where stars are honored, and Griffith Observatory, offering stunning views of the city and the Hollywood sign. The Getty Center showcases world-class art, while Universal Studios Hollywood brings movies to life.
Nearby, Beverly Hills shines with luxury, and Santa Monica offers the iconic Santa Monica Pier. Long Beach features a beautiful waterfront, and Pasadena is known for its historic architecture and the Rose Bowl. Whether you’re exploring beaches or famous sites, Los Angeles has something to offer everyone.
We Will Verify Your Insurance for Treatment
Inpatient Depression and Addiction Treatment
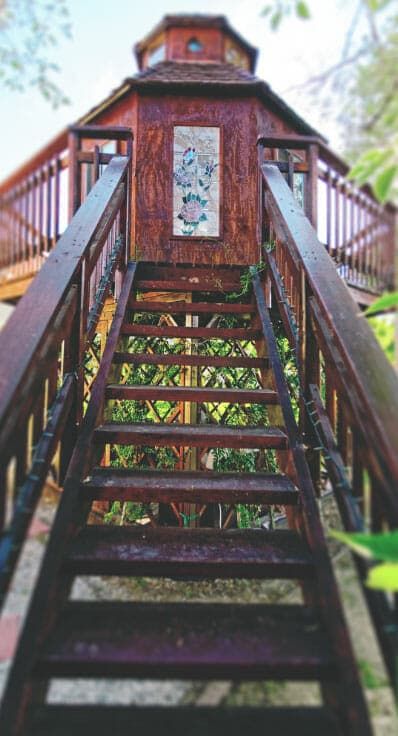
Inpatient treatment for depression and addiction focuses on addressing two interwoven challenges—depression and substance dependence—in a safe and structured environment. At Harmony Place in Woodland Hills, CA, this dual-diagnosis approach is specifically tailored to meet the needs of individuals facing these complex struggles. Depression often leads to self-medicating with substances, while addiction can intensify feelings of hopelessness and isolation, creating a destructive cycle. The inpatient programs at Harmony Place prioritize stabilization, providing round-the-clock care, evidence-based therapies, and close monitoring in a nurturing setting. By identifying and addressing underlying issues, this treatment model helps clients gain clarity and build a strong foundation for sustained recovery.
Harmony Place creates a focused space to manage depression alongside alcohol or drug addiction through individualized care plans and holistic support. For those combating alcohol addiction, the inpatient program includes supervised medical detoxification, therapeutic techniques to address emotional pain, and tailored strategies for healthy coping mechanisms. Similarly, clients recovering from drug addiction benefit from a combination of psychiatric care, group support, and life skills development to address triggers and prevent relapse. Located in the serene neighborhood of Woodland Hills within Los Angeles, Harmony Place offers a tranquil and restorative backdrop, making it an ideal setting for individuals to fully commit to healing and regaining control of their lives.
Outpatient Depression and Addiction Treatment
Outpatient depression and addiction treatment offers a flexible solution for individuals dealing with the dual diagnosis of mental health struggles and substance use issues. At Harmony Place in Woodland Hills, CA, outpatient programs are crafted to meet the unique needs of each client while allowing them to maintain their daily routines. Depression often overlaps with alcohol or drug dependency, making recovery a highly individualized process. Through tailored therapy sessions, clients uncover the underlying causes of these interconnected challenges. This approach fosters emotional stability and helps individuals overcome their dependency in a manageable, supportive setting. Clients can receive high-quality treatment without needing to leave their professional, educational, or personal commitments behind.
At Harmony Place, the outpatient program is designed to address depression alongside alcohol or drug addiction with a comprehensive, compassionate approach. For those recovering from alcohol addiction, treatment includes targeted counseling and relapse prevention techniques aimed at breaking the connection between depressive symptoms and drinking. Similarly, for individuals overcoming drug addiction, the focus is on stabilizing mental health while addressing addiction cravings and relapse triggers through integrative care. Conveniently located in Woodland Hills, within the Los Angeles area, Harmony Place provides a well-balanced environment where individuals can find support, growth, and recovery. With a commitment to flexible care and expert guidance, Harmony Place empowers its clients to take charge of their mental health and begin lasting recovery.
Can a Drug or Alcohol Addiction Cause Depression Disorders?
Yes, addiction can cause depression. When you struggle with substance misuse or alcohol abuse, the effects on your brain and body can lead to feelings of hopelessness or sadness and a lack of motivation. You may find yourself asking, “Can drug addiction cause depression?” The answer is yes; the two conditions often go hand in hand.
Substance abuse can disrupt your brain chemistry and exacerbate existing mental health issues, making depression more likely. Additionally, the stress and challenges of substance addiction can further contribute to depressive symptoms. Addressing both addiction and depression simultaneously is crucial for effective treatment and lasting recovery. If you’re facing these challenges and asking yourself, “Can addiction cause depression?” seeking help is the first step toward healing. Reach out to Harmony Place Drug and Alcohol Treatment to find out how our substance abuse therapy and holistic approaches to depression treatment can help.
Can Depression Disorders Lead to Addiction and Substance Abuse?
Yes, depression can lead to addiction and substance abuse. When you experience depression, you might seek out substances like alcohol or drugs to numb emotional pain or escape from feelings of sadness and hopelessness. This self-medication can quickly spiral into addiction as you use substances more frequently to cope with your symptoms.
There is a complex relationship between conditions like depression and substance abuse, with each condition potentially worsening the other. Addressing both depression and addiction is crucial for effective treatment, relapse prevention, and long-term recovery.
Signs and Symptoms of Co-Occurring Depression and Substance Addiction
Recognizing the signs and symptoms of both substance abuse and depression is essential for seeking timely help and achieving recovery. These conditions often overlap, making it crucial to identify the indicators that might suggest a dual diagnosis. Understanding these signs can help you or a loved one get the support needed for effective treatment.
Common Signs and Symptoms of Depression
Typical signs and symptoms of depression include persistent feelings of sadness or hopelessness that don’t seem to go away. You might notice a lack of interest in activities you once enjoyed or difficulty concentrating on daily tasks. Changes in sleep patterns, like insomnia or sleeping too much, are also common.
You may experience changes in appetite, either eating too much or too little, and feel tired or low on energy. Physical symptoms like unexplained aches and pains can occur, and you might struggle with feelings of worthlessness or guilt. If you recognize these signs in yourself, seeking out professional help is crucial for managing and overcoming depression effectively.
Common Signs and Symptoms of SUDs
Being able to recognize the symptoms of substance use disorders (SUDs) is crucial for getting help and making positive changes. These indicators can help you identify if you or someone you care about might be struggling with addiction. Understanding these symptoms can guide you in finding the right support and treatment to address the issue effectively.
- Cravings: You may experience intense urges or desires to use the substance, making it hard to focus on anything else.
- Tolerance: You might need more substance over time to achieve the same effect, signaling your body has built up tolerance.
- Withdrawal: When you try to stop or cut back, uncomfortable physical or emotional symptoms like anxiety, nausea, or irritability may arise.
- Neglecting responsibilities: You may begin to neglect work, school, or family obligations due to substance use.
- Loss of Control Over Substance Use: Even if you want to cut back, you may find it difficult to stop using the substance.
- Continued Use Despite Negative Consequences: You keep using the substance even when it leads to health, legal, or relationship problems.
- Social Isolation: You might withdraw from family, friends, or social activities as substance use takes priority.
- Risky Behavior: Engaging in dangerous actions, like driving under the influence, becomes more frequent.
- Physical Health Issues: Long-term use of some substances can lead to liver damage, heart disease, or other medical conditions.
- Mood Swings: Extreme changes in mood or irritability are often linked with substance abuse.
What Are the Co-Occurring Risks of Substance Addiction and Depression Disorders?
When you’re dealing with both substance addiction and depression, you face a range of co-occurring risks that can severely affect your life. Understanding the risks is crucial for recognizing the seriousness of your situation and seeking appropriate help. Here are some common risks associated with co-occurring substance addiction and depression disorders.
- Increased Risk of Overdose: Combining substance abuse with depression can heighten the risk of overdose, as the body’s ability to process substances is compromised.
- Worsening Mental Health (Depression and Anxiety): The presence of a mental health diagnosis and co-occurring substance abuse can intensify symptoms, making depression and anxiety more severe and harder to manage.
- Higher Suicide Risk: The combination of addiction and depression increases the risk of suicidal ideation or actions due to overwhelming emotional pain and hopelessness.
- Severe Physical Health Decline: The dual effect of substance abuse and depression can lead to serious health problems, including chronic diseases and weakened immune function.
- Strained Relationships and Social Isolation: Addiction and depression often lead to withdrawal from loved ones, causing relationships to suffer and increasing social isolation.
- Impaired Cognitive Function: Both disorders can affect your memory, capacity for decision-making, and your ability to think clearly, affecting daily functioning.
- Legal and Financial Problems: Substance abuse can lead to legal issues and financial strain, further compounded by the challenges of managing depression.
- Difficulty Maintaining Employment: The combined effects of addiction and depression can make it challenging to keep a job or perform well at work.
- Aggressive or Risky Behavior: Substance use and depression can lead to impulsive, risky, or aggressive behaviors that put you and others at risk.
Co-Occurring Depression and Substance Addiction Facilities Near Me in Los Angeles, CA
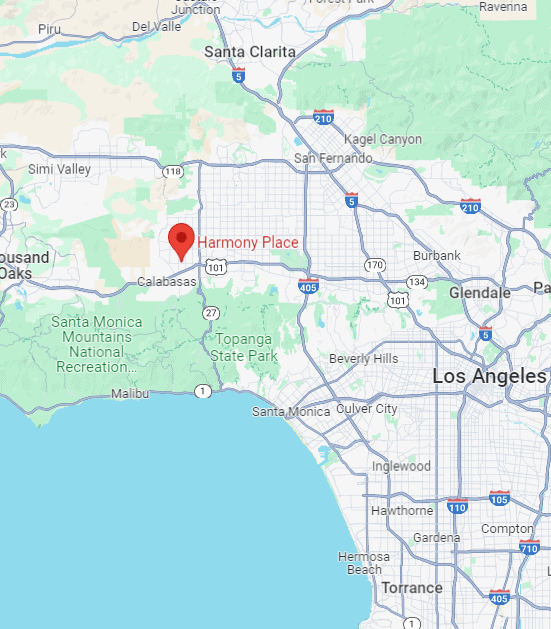
At Harmony Place’s rehab center in Los Angeles, CA, we provide specialized concurrent depression and substance abuse treatment. Our comprehensive programs are tailored to your needs, offering the support and care necessary for lasting recovery. Whether you require outpatient care, inpatient rehab, or a combination of therapies, contact us at (855) 652-9048 to discuss our dual-diagnosis treatment options.
Outpatient Depression and Addiction Rehab Facility Near Me
If you’re searching for an outpatient depression and addiction rehab facility “near me,” Valley Restoration Center in Woodland Hills, CA, offers a compassionate and flexible option for recovery. Conveniently located at 22900 Ventura Blvd., Ste. 314, our center specializes in treating individuals managing the dual challenges of depression and substance use. Outpatient programs are designed to fit into your daily routine, empowering you to maintain your work, education, or family responsibilities while receiving care. Our team provides evidence-based therapies tailored to your specific needs, creating a supportive path toward emotional balance and freedom from substance dependency.
Valley Restoration Center’s outpatient services focus on addressing the complex relationship between depression and addiction, particularly drug dependence. Through personalized therapy sessions, clients work to identify the root causes of their struggles, learning practical and sustainable coping strategies. Individual counseling, group support, and relapse prevention techniques form the foundation of this program. The flexibility of outpatient care allows clients to actively participate in their recovery while continuing to engage with their local community. Our facility accepts multiple insurance plans, helping to remove financial barriers and ensuring access to effective treatment for individuals and families in the Woodland Hills and Los Angeles areas.
Located on Ventura Blvd., Valley Restoration Center is easy to reach for clients throughout San Fernando Valley and nearby communities like Tarzana, Encino, and Calabasas. The center is a short drive from the Ventura Freeway (US-101) for those traveling by car, and it’s also accessible via public transport, with nearby bus routes connecting you to our location. Our serene and welcoming environment in Woodland Hills offers the perfect backdrop for outpatient care, blending convenience with privacy to help clients focus on their healing. If you’re looking for a professional, supportive outpatient program “near me,” Valley Restoration Center is here to help you take meaningful steps toward lasting recovery.
Inpatient Depression and Addiction Rehab Facility Near Me
If you’re searching for an inpatient depression and addiction rehab facility “near me,” Harmony Place in Woodland Hills, CA, offers a sanctuary for healing and recovery. With two convenient locations—Harmony Place at 23041 Hatteras St. and Harmony Place East at 22913 Burbank Blvd.—our facilities are equipped to support individuals facing the dual challenges of mood disorders and substance dependence. Depression and addiction often intertwine, creating a need for comprehensive care that addresses these struggles simultaneously. At Harmony Place, we offer round-the-clock professional support, evidence-based therapies, and a structured environment to help you or your loved one regain emotional stability and break free from substance use.
Our inpatient programs focus on healing the effects of depression while also addressing either alcohol or drug addiction in a holistic manner. Clients struggling with alcohol dependency benefit from services like supervised detoxification, medication support, and individualized therapy to address both chemical dependency and the emotional pain that often accompanies depression. For individuals living with drug addiction, the approach combines psychiatric care, coping strategies, and relapse prevention techniques, ensuring that recovery addresses both mind and body. With an emphasis on dual-diagnosis treatment, our dedicated team works to uncover the root causes of depression and addiction, building a foundation for sustainable health and wellness.
Harmony Place’s two locations in Woodland Hills are ideally situated for accessibility and tranquility. Nestled in the heart of this serene Los Angeles neighborhood, the facilities are a short drive from Ventura Blvd. and the Ventura Freeway (US-101), offering easy access for individuals throughout the San Fernando Valley and greater Los Angeles areas. Public transit options, including local bus routes, connect nearby, making the centers reachable for those without a personal vehicle. Combined with the peaceful, restorative surroundings of Woodland Hills, Harmony Place provides a setting where clients can focus solely on their recovery, knowing they are receiving top-quality care close to home. For anyone searching for inpatient addiction and depression treatment “near me,” Harmony Place is here to support you every step of the way.
What to Look for in a Dual Diagnosis Treatment Recovery Center
Being diagnosed with a depressive disorder is not a death sentence, with the right care and guidance, most people get back on their feet and live their lives to the fullest. Finding the treatment center that best suits one’s needs is also as important as seeking help on time.
There are some things to bear in mind when trying to decide where to receive therapy. Some of these things are:
- The qualification of staff members at the treatment center
- The types of therapy for therapy and counseling for depression that are provided
- If they offer an individualized inpatient depression treatment program
- The level of involvement of the patients and their families with the inpatient depression treatment program

At Harmony Place, we strive to provide the best inpatient depression treatment center in the Los Angeles area. Our clients can recover in a safe, inclusive, and affordable environment.
Does Health Insurance Cover Dual Diagnosis Treatment for Addiction and Depression Disorders in LA?
Yes, private health insurance often covers treatment for both addiction and depression in Southern California. Coverage can vary by plan and provider, but many policies include options for inpatient and outpatient services, therapy, detoxification, supportive counseling, and antidepressant medications like selective serotonin reuptake inhibitors (SSRIs). To understand your benefits fully, reviewing your policy and contacting Harmony Place is important.
The Harmony Place Treatment Center team can provide details on what treatments are covered, any out-of-pocket costs, and how to access the services you need. If you’re unsure about your coverage or need assistance, don’t hesitate to reach out to us for clarification and support in navigating your mental health treatment and addiction intervention options.
How Much Does a Dual Diagnosis Program for Depression Treatment Cost in Los Angeles, CA?
The cost of dual diagnosis substance abuse and depression treatment in greater Los Angeles can vary widely depending on the type of facility and level of care. On average, you might expect to pay between $10,000 and $30,000 for a 30-day inpatient program. Outpatient programs generally cost less, ranging from $5,000 to $15,000 for a similar period.
These estimates can fluctuate based on factors like the specific treatment center, care intensity, and insurance coverage. To get a more accurate cost estimate tailored to your needs and insurance plan, it’s best to contact Harmony Place at (855) 652-9048. We can provide detailed information on costs and payment, as well as information on our depression screening and substance abuse treatment options.
How to Get into Dual Diagnosis Rehab for Recovery Treatment in LA
To get into rehab for depression and substance addiction, start by reaching out to treatment centers like Harmony Place to discuss your needs and available options. Begin by researching facilities specializing in dual diagnosis, as they simultaneously address both conditions.
Contact Harmony Place to inquire about our programs, treatment approaches, and admission process. If you have insurance, check your coverage to understand what costs are covered and whether the facility accepts your plan. You’ll likely need to undergo an intake assessment to determine the appropriate level of care. By taking a free assessment, it will give us a good idea on how to approach your condition. This helps ensure you receive the support you need for effective recovery.
Comprehensive Dual Diagnosis Rehab in California
Harmony Place in Los Angeles provides comprehensive treatment for clients with Dual Diagnosis conditions. Our programs treat mental health and substance use disorders simultaneously, focusing on trauma, PTSD, anxiety, depression, bipolar disorder, and ADHD. We help clients restore balance through integrated, evidence-based therapies in Southern California.
- Inpatient Rehab Los Angeles
- Intensive Outpatient Program Los Angeles
- Evening Intensive Outpatient Program
- Medication Assisted Treatment Los Angeles
- Outpatient Rehab Program Los Angeles
- Los Angeles Partial Hospitalization Program
- Medically Assisted Detox LA
- Sober Living Homes and Halfway Houses
- Clinical Care Los Angeles
- Family Therapy Rehab Program
- Couples Rehab Los Angeles
- Men’s Addiction Rehab California
- Women’s Rehab Center SoCal
- Addiction Treatment for Veterans
- Short-Term Addiction Rehab
- Long-Term Addiction Rehab
- Private Luxury Rehab Los Angeles
- Faith-Based Rehab Programs
- Non-Faith-Based Rehab
- Rehab for Professionals LA
- Rehab Aftercare Alumni Programs
California Addiction Treatment and Depression Statistics and Information
- From Feb. 1 to 13, 2023, 31.7% of California adults reported experiencing symptoms of anxiety and/or depressive disorder, KFF reported.
- In 2019, 58.5% of California’s substance use disorder treatment facilities offered programs designed for those with both co-occurring mental illness and substance use disorders, according to the California Health Care Foundation.
- 19.3% of U.S. adults, or 9.2 million people, who had a mental illness also had a substance use disorder in 2018, according to NAMI California.
- 931 substance use treatment facilities treated clients diagnosed with co-occurring mental health conditions and substance use disorders, according to the 2022 National Substance Use and Mental Health Services Survey by the Substance Abuse and Mental Health Services Administration (SAMHSA).
- Mental Health America ranked California 16th lowest in the U.S. for prevalence of mental health and substance use










